 I was never the nurse who followed the rules.
I was never the nurse who followed the rules.
I don’t believe that you can fit patients into a box. Every person is unique, every illness is different, every disease process individual, every history rare and every healthcare setting distinct.
Working in both Australia and England I often felt strangled by so many rules and regulations. There are best practice guidelines, clinical guidelines, flow charts, standards and care plans, scales, scores, and values, directives, risk assessments and protocols. Clinical governance, incident management, risk reporting, performance management and reflective practice are all terms at which I would let out a heavy sigh and role my eyes. Don’t we have enough do? Is it not just another form, meeting or discussion to add to the already heavy load?

I often felt frustrated by these guidelines. Nurses live in fear of differentiating from the norm. Working in a remote healthcare setting, I often had to think outside the box, to adjust the rules, to fly by the seat of my pants. Words such as negligence, compensation, accountability, misconduct and scope of practice constantly hung over my head, keeping me awake at night. Of course we always want to do what is best for our patients, but during the rush of the trauma with the adrenaline pumping, mistakes do happen, bad decision are sometimes made. Nobody wants to end up in court for trying to save a life.
Now, imagine a world where there are no rules, there are no regulations. Imagine a world where accountability and responsibility cease to exist.
Imagine a job where getting to work an hour, maybe two hours late every day is acceptable. Imagine a job where sleeping, smoking and getting high during work hours is the norm, where lunch breaks last for hours and the only thing you ever read is the newspaper. Imagine a job where you will never get a verbal or written warning and it is virtually impossible to get fired. Would you really want to work there?
What if you have been a nurse for more than 10 years and you only had the original knowledge base from that first diploma you ever did? What if you had never had a mentor or anybody who ever questioned what or why you do the things that you do? Would your practice be current? Your skills be up-to-date?
Would you be able to justify not giving a lifesaving drug for over 8 hours because you didn’t understand what it was for? Or would you want to find out? If you didn’t have the equipment you needed to carry out basic observations and nursing interventions, wouldn’t you jump up and down, shout until you got it?
Imagine dealing with so much illness and death, day in, day out, knowing that most of the time it is avoidable, yet not knowing what you need to do or what you can do improve the situation. Imagine if death was the norm and not the exception. Would you cease to care? Wouldn’t you want to talk about it? To work out what you need to know, to try to find solutions, to ensure that the next patient at least has a chance of survival?
Now, think about turning up to an emergency department with your sick child in the middle of the night. After two hours, you are told that that there is no nurse because the previous shift left early. After four hours you are told there is still no nurse because the late shift has not yet arrived. You would want somebody to be held responsible for that. Wouldn’t you?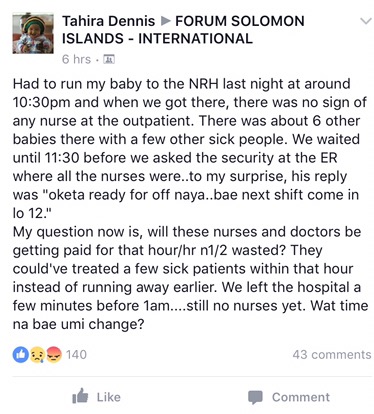
Do you know what it creates: A world without accountability and responsibility, without rules and regulations, policies and procedures? It creates a world that is stuck in a time warp. Nothing ever changes. If we don’t reflect on what we do and why things happen then we never see that anything is wrong. If we can’t see that anything is wrong, then why would we try to change it? So it never changes. We make the same mistakes, people continue to die unnecessary deaths and the world just keeps on spinning, day after day, week after week, year after year.
So bring on the paperwork! Bring on the clinical governance! Bring on reflective practice! I am a converted nurse. And I never thought I would ever hear myself saying that.
It has taken me over seven months to realise the extent of the problem. On the surface, things just seem to tick along nicely. I knew there were concerns but I was only being shown the tip of the iceberg. So, me, being typical me, spent a week falling apart. Of course, I think it is all my responsibility: What should I do to right this wrong that has taken developed countries decades to rectify? (Have they?) How can I introduce new systems in the blink of an eye that have taken panels, councils, unions, boards and committees of trained professional’s a lifetime to develop? Where do I find the money, the time, the expertise, the technology and the equipment needed to ensure that education and evidence based practice is delivered in all aspects of care? Can I single handedly, in four months, teach years of experience in every clinical area?
 Can I remove cultural norms and expectations, break down years of barriers and behaviors and replace them with a different set of motivations and ethics? Can I do it by PowerPoint?
Can I remove cultural norms and expectations, break down years of barriers and behaviors and replace them with a different set of motivations and ethics? Can I do it by PowerPoint?
No. Is the answer. And nobody expects me too. Sometimes the truth is harder to deal with than the expectation but of course, no one person could ever make that amount of difference in one year to a whole hospital, no matter where it was, and especially not here. I am gradually becoming OK with that, but it is hard, to know that so many deaths could be avoided. So, I guess I’ll just carry on doing what I’m doing. Bit by bit. In a calm and relaxed manor.

Last night, over dinner, I was discussing my thoughts and feelings with my new mate: pocket rocket Kate and she said to me (in her terrible Kath and Kim Aussie accent) “yeah mate, I see what you’re saying, but have you noticed that nobody is that unhappy? Nobody is stressed to the eyeballs, lying awake at night, thinking about what they did or didn’t do at work. Nobody goes home, consumed with anger that their boy should have lived. They just think it is God’s way. He died of natural causes and he was cared for till the end”.
She is right.
The Solution? Who knows? I doubt we will find it in my life time but I’m guessing there must be a happy medium somewhere between the two systems. A place where we learn and grow from the mistakes we make but where we do not need to sacrifice our wellbeing and happiness for fear of doing the wrong thing.










And in the middle of all that isn’t there a road to best practice in the growth of an out-of-system practice? We all know the burdens (as well as benefits) of true reporting and best practice. In a fully developed system the drill-down available into that data allows all kinds of improvement as the findings are applied, but we also understand the level of governance it takes to deliver that kind of improvement etc. I have no idea if i’m wrong or right but i do know that in a results-based role action and hands-on time are the key ingredients in ensuring the delivery or non-delivery within that role. Surely, without the administrative system around you and budgets granted for delivery not research the delivery has to be within a paradigm that takes the reality, not best practice of developed systems into account. Following on from this, there then needs to be an ever-so-efficient practice of identifying and disseminating relevant new developments and practice so as to have most impact. There’s got to be something regarding the 80:20 rule applicable here which supports the optimal balance between saving lives and health, and researching / employing more efficient ways to do that. How do medicins sans frontiers do it and do they have a transition path from emergency to longer-term community support. This has bugged me for a while, especially when you look at places like haiti (as they’re still stuck in emergency as there’s no emerging healthcare process and the funds haven’t been delivered). I suppose africa would have some good examples of innovative solutions and practice as the country has been through so much with current examples of systems that work that have been built from intervention-type responses. Sounds like you need to write your own best practice for a relatively non-documented case. Just a thought Anna.
My heath service saved my life. Everyone deserves it 🙂
LikeLike
Or maybe it is well documented i don’t know, but it doesn’t sound like you have the documents 🙂
LikeLike
Hi Anna I have now finished reading your blog and wanted to say how wonderful it’s been to read so interesting a story,see such amazing pics. and what a fantastic writer you are. You are taking after your Dad! Glad you are back in civilisation though as you had me worried more than once !! lots of love, Juliaxxxx
LikeLike